Understanding Epilepsy: Causes, Symptoms, and Treatment Options
Epilepsy functions as a neurological condition that disrupts brain electrical patterns in multiple people throughout the world triggering unprovoked seizure activity. People with this disorder experience symptoms that vary from gentle to intense seizures which affect their ability to function normally. The medical community cannot identify the exact causes of epilepsy since this neurological disorder can develop from brain injuries as well as genetic predisposition or developmental disorders.
What is Epilepsy?

The recurrent seizures that occur in epilepsy constitute a continuous neurological disorder. The severity and frequency of seizures as well as their symptoms depend on which part of the brain the seizures originate from. Epilepsy emerges most frequently in children along with people from older age groups.
Causes of Epilepsy:
Epilepsy can arise from a variety of factors, including:
1. Genetic Predisposition
Some individuals inherit a genetic tendency toward epilepsy. If a close family member has the condition, the likelihood of developing epilepsy may be higher.
2. Brain Trauma
Head injuries caused by accidents, falls, or sports-related impacts can trigger epilepsy, especially in cases of severe brain trauma.
3. Infections and Medical Conditions
The brain becomes inflamed after meningitis or encephalitis infection which can subsequently trigger epilepsy. Brain-related health conditions among the population effectively contribute toward the development of epilepsy.
4. Developmental Disorders
Epilepsy has a higher incidence rate within patients suffering from autism and cerebral palsy among other neurological diseases. Patients who experience such conditions often develop abnormal brain workings which results in seizure activation.
5. Prenatal and Birth Complications
Brain damage caused by oxygen deprivation, infections during pregnancy, or complications during childbirth can increase the chances of developing epilepsy later in life, whether during childhood or adulthood.
Recognizing Common Symptoms of Epilepsy:
Epilepsy is primarily identified by seizures, though their type and intensity can differ greatly. Here are some of the most common symptoms to be aware of:
Convulsions and Uncontrolled Movements
Seizures often lead to involuntary jerking movements in the arms and legs. In some cases, they may cause muscle stiffness or a complete inability to move.
Loss of Consciousness
A temporary loss of awareness or consciousness is a frequent occurrence during seizures for many individuals with epilepsy.
Sensory Abnormalities
Seizures can trigger unusual sensations, such as tingling, flashes of light, or detecting smells that aren’t actually present.
Emotional and Cognitive Shifts
Confusion, fear, anxiety, or brief memory loss may occur before, during, or after a seizure, often adding an emotional or mental dimension to the experience.
Repetitive Movements
Certain seizures manifest as repetitive actions, such as blinking, lip-smacking, or hand gestures, typically performed without the person being aware of them.
Types of Seizures:
Seizures are classified into two main categories:
1. Focal Seizures
These seizures begin in a specific region of the brain and can trigger localized symptoms, such as muscle twitching in a single limb or sensory disruptions.
2. Generalized Seizures
These seizures affect both sides of the brain and include different types such as:
- Tonic-Clonic Seizures: Involve loss of consciousness, stiffening, and jerking movements.
- Absence Seizures: Cause brief lapses in awareness, often mistaken for daydreaming.
- Myoclonic Seizures: Result in sudden, brief muscle jerks.
- Atonic Seizures: Cause a sudden loss of muscle tone, leading to falls.
Diagnosing Epilepsy:
Accurate diagnosis of epilepsy requires a comprehensive medical evaluation, which typically includes the following steps:
Medical History and Symptom Analysis
The diagnostic process begins with a comprehensive review of the patient’s medical history. Physicians focus on the type, frequency, and potential triggers of seizures, while also inquiring about family history of epilepsy, past illnesses, or head injuries that may be relevant. This thorough assessment is crucial for identifying patterns, understanding the condition, and crafting a treatment plan tailored to the patient’s unique needs.
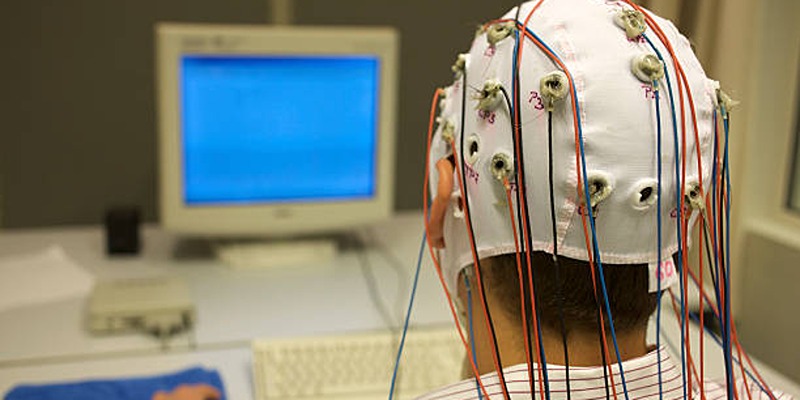
Electroencephalogram (EEG)
An EEG is a non-invasive test that monitors the brain’s electrical activity using electrodes placed on the scalp. It identifies abnormal brain wave patterns, such as spikes often linked to epilepsy. Conducting an EEG during or soon after a seizure provides the most accurate data, making it an essential tool for confirming an epilepsy diagnosis.
Imaging Tests (MRI and CT Scans)
Advanced imaging technologies, including MRI and CT scans, produce detailed images of the brain. These scans can uncover structural issues such as tumors, brain injuries, or congenital abnormalities that may be causing seizures. In some cases, imaging can pinpoint specific brain regions involved in seizure activity, providing critical insights for treatment planning, including surgical options when necessary.
Blood Tests
Blood tests help uncover potential underlying causes of seizures, such as infections, metabolic disorders, autoimmune diseases, or genetic conditions associated with epilepsy. They also help identify imbalances or deficiencies that might contribute to seizure activity, allowing doctors to exclude other conditions that mimic epilepsy.
Epilepsy Treatment Options:
While epilepsy may not always have a cure, it can often be effectively managed through appropriate treatment. Here are the most common approaches:
1. Medication Therapy
Antiepileptic drugs (AEDs) are the cornerstone of epilepsy treatment, offering the most effective way to control seizures for the majority of patients. These medications work by modulating electrical activity in the brain, reducing the likelihood of seizures. The choice of an AED depends on factors such as seizure type, the patient’s age, medical history, and potential side effects.
2. Surgical Treatments
For individuals whose seizures cannot be controlled with medication, surgical intervention may offer a solution. Procedures like lobectomy, where the seizure-causing part of the brain is removed, or corpus callosotomy, which disconnects communication between brain hemispheres, aim to reduce or eliminate seizures. These surgeries are typically considered only after extensive testing, including imaging and seizure mapping, to ensure they are safe and suitable for the patient.
3. Vagus Nerve Stimulation (VNS)
Vagus Nerve Stimulation (VNS) is a viable treatment option for patients who do not respond to medications and are not candidates for surgery. A small device is surgically implanted in the chest and connected to the vagus nerve in the neck. This device delivers regular electrical impulses that can help reduce the frequency and severity of seizures. Over time, VNS has been shown to enhance patients’ quality of life by decreasing seizures and stabilizing mood.
4. Ketogenic Diet
The ketogenic diet is a specialized dietary therapy designed to manage drug-resistant epilepsy, particularly in children. This high-fat, low-carbohydrate diet shifts the body into a metabolic state called ketosis, which has been proven to lower seizure frequency. The diet is carefully customized and monitored by healthcare professionals to meet individual nutritional needs.
Living with Epilepsy:

With proper management, individuals with epilepsy can live full and meaningful lives. Effective epilepsy care involves several key practices:
- Consistent Medication Use: Taking prescribed medications as directed to help control seizures.
- Recognizing Triggers: Identifying and avoiding potential seizure triggers, such as sleep deprivation, high stress levels, or certain environmental factors.
- Routine Medical Care: Regular checkups to monitor seizure patterns and adjust treatments as needed for optimal management.
- Emergency Readiness: Ensuring family and friends understand how to provide assistance during a seizure.
Conclusion
Epilepsy is a complex neurological condition, but with the right treatment and lifestyle adjustments, it is possible to manage seizures and maintain a healthy, balanced life. Raising awareness about its causes, symptoms, and treatment options is crucial for empowering those affected and fostering a more supportive environment.