Recognizing the Warning Signs of Henoch-Schonlein Purpura: All You Need to Know
The rare disorder Henoch-Schonlein Purpura (HSP) compromises blood vessels. Though it can also strike adults, it is most frequent in youngsters. The illness inflames the tiny blood vessels, which results in symptoms in the kidneys, digestive tract, skin, and joints. Timely treatment depends on an awareness of its early warning symptoms. Although the precise reason for HSP is uncertain, it usually follows infections.
Typical triggers are allergies, some medications, or even respiratory problems. Early identification can avoid difficulties. The first signs are often a rash, stomach trouble, and joint swelling. This article will discuss the main HSP symptoms and indicators. We will also cover diagnosis, available treatments, and complications of HSP.

What Is Henoch-Schonlein Purpura?
Small blood vessels in the autoimmune disorder Henoch-Schonlein Purpura (HSP) become inflamed. This inflammation can cause bleeding and damage to many organs, including the skin, kidneys, joints, and gastrointestinal tract. Following an infection—such as a cold, sore throat, or upper respiratory illness—HSP sometimes results. Though it can occasionally strike adults, the disease most usually strikes children between the ages of two and eleven.
Boys acquire HSP somewhat more often than girls do. While most cases are clear on their own without major consequences, some people may have more severe problems, including gastrointestinal problems or renal damage. HSP is categorized as vasculitis, in which case blood vessels swell. Management of symptoms and avoidance of consequences depend on early detection and medical treatment.
Key Warning Signs of HSP
Below are the key warning signs of Henoch-Schonlein Purpura (HSP) to help identify and manage the condition effectively.
- Skin Rash: HSP first manifests itself as a characteristic rash. The rash usually appears on the skin as purple or red dots. These patches are usually on the legs, buttocks, and lower body. The rash could seem like elevated patches or little bruises. It arises from blood vessels' bleeding from inflammation. Severe cases could cause the rash to develop in other body parts.
- Abdominal Pain: Another often-occurring HSP symptom is stomach trouble. It is brought on by digestive system blood vessel irritation. Usually mimicking cramps, the pain could be minor or severe. At times, it causes diarrhea, nausea, or vomiting. Rarely blood shows up in the stool.
- Joint Pain and Swelling: HSP frequently results in joint pain and swelling, especially in the knees and ankles. The suffering can impede mobility and influence daily tasks. This symptom is usually transient and goes away when the illness gets better. However, the afflicted person may find it rather uncomfortable.
- Fever and Fatigue: Fever and tiredness are also common general symptoms in HSP. These complaints point to continuous inflammatory activity within the body. Although they might not seem particular, they usually use other warning signals. By tracking these symptoms, one can help spot the illness early on.
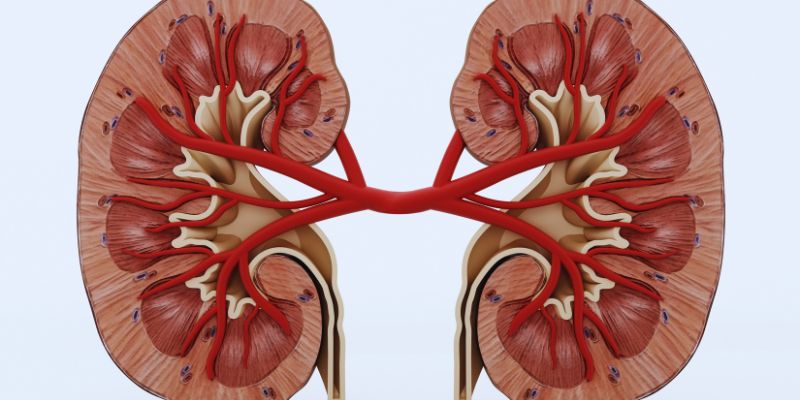
- Kidney Problems: One major problem of HSP is kidney involvement. It could cause protein or blood to appear in the urine. Sometimes, this results in swelling in the legs, feet, or face. If untreated, kidney issues could develop into more severe diseases. Frequent urine tests enable one to check one's kidney condition.
How Is HSP Diagnosed?
Henoch-Schonlein Purpura (HSP) is diagnosed through physical exams, medical history reviews, and specific tests. Throughout the exam, Doctors search for typical symptoms such as purplish rash, joint swelling, and stomach pain. These outside symptoms often provide important hints for the diagnosis of the disorder. Finding kidney involvement mostly depends on urine tests. Their search for blood or protein in the urine suggests possible renal injury.
Blood tests also evaluate signs of inflammation, such as increased white blood cell counts, and help to rule out other probable disorders. Under rare or more severe circumstances, doctors could advise a biopsy. A little tissue sample from the kidney or skin is examined under a microscope to verify the diagnosis. Managing HSP and avoiding consequences, including kidney disease, depends on timely diagnosis.
Treatment Options for HSP
Below are the treatment options for Henoch-Schonlein Purpura (HSP) that can help manage symptoms and prevent complications effectively.
- Symptom Management: Most cases of HSP pass on their own without particular treatment. However, controlling symptoms will help to increase comfort. For joint suffering, doctors could advise over-the-counter painkillers. Rest and water are also absolutely vital during recuperation.
- Medications: In severe cases, patients may need prescription medications like corticosteroids. These medications control problems and aid in lowering inflammation. People with kidney issues could need other medications, such as medications meant to reduce blood pressure or immunosuppressants.
- Supportive Care: Rarely occurring severe HSP may call for hospitalization. It guarantees close observation and handling of complications in therapy. Doctors might offer intravenous fluids, painkillers, or other supporting treatment as necessary.
Complications of HSP
Although most cases of Henoch-Schonlein Purpura (HSP) go away without any consequences, occasionally, problems arise. Damage to the kidneys is the most major issue since it could lead to long-term conditions, including chronic kidney disease. Kidney problems are often indicated by symptoms such as swelling (edema), dark-colored urine, or blood or protein in the urine. Another possible problem is intussusception, a disorder whereby one section of the intestine slides into another.
Severe stomach pain, vomiting, or even bowel blockage brought on by this calls for quick medical attention. Rarely, especially if renal involvement is left untreated, HSP can cause more severe results, including kidney failure or ongoing high blood pressure. Management of HSP and lower risk of consequences depend on early therapy and prompt diagnosis—frequent visits to a healthcare professional guarantee close monitoring of symptoms and resolution of any developing problems.
Conclusion:
In conclusion, mostly in youngsters, Henoch-Schonlein Purpura (HSP) is an uncommon autoimmune condition impacting tiny blood vessels. Diagnosis and treatment delay depends on early recognition of symptoms, including rash, stomach ache, joint swelling, and possible kidney problems. Although most cases are clear, problems might arise, including intestinal blockage or renal damage. Appropriate treatment, frequent monitoring, and quick medical response will help control symptoms and stop major outcomes. Better health outcomes and reduced long-term hazards for those living with HSP depend on an awareness of the disorder and its warning signals.